Vice president of pharmacy benefits management at GreenShield highlights weight management drugs are having the most impact on Canadian healthcare

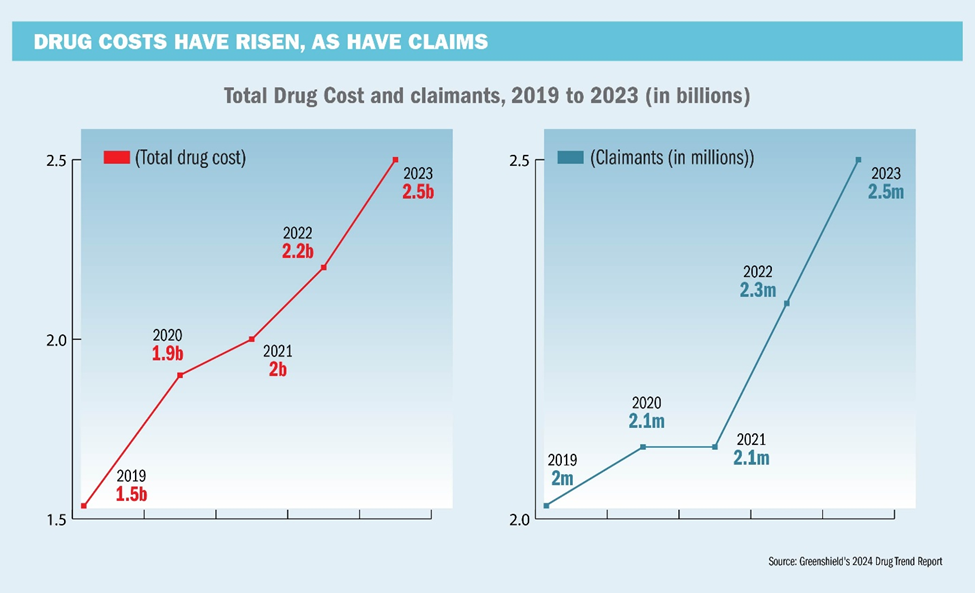
It can feel hard to be a Canadian right now. Cost of living remains extremely elevated and many Canadians are grasping to make ends meet before year end. A reflection of the current economy, GreenShield’s recent 2024 Drug Trends Report found that drug costs are also up 11 per cent, year-over-year. Since 2019, total drug costs adjudicated by GreenShield have risen from about $1.55 billion to $2.46 billion in 2023. At the same time, the number of claimants has increased from 2.0 million to 2.5 million. Last year, the cost per claimant reached an all-time high of $971.
For plan sponsors, the findings present an opportunity to reassess benefits offerings and drug coverages. Ned Pojskic, GreenShield’s vice president of pharmacy benefits management highlights the significant patterns shaping healthcare and drug benefits in Canada. The findings emphasize how the rising prevalence of chronic diseases, advances in high-cost medications, and evolving treatment models are transforming the healthcare landscape.
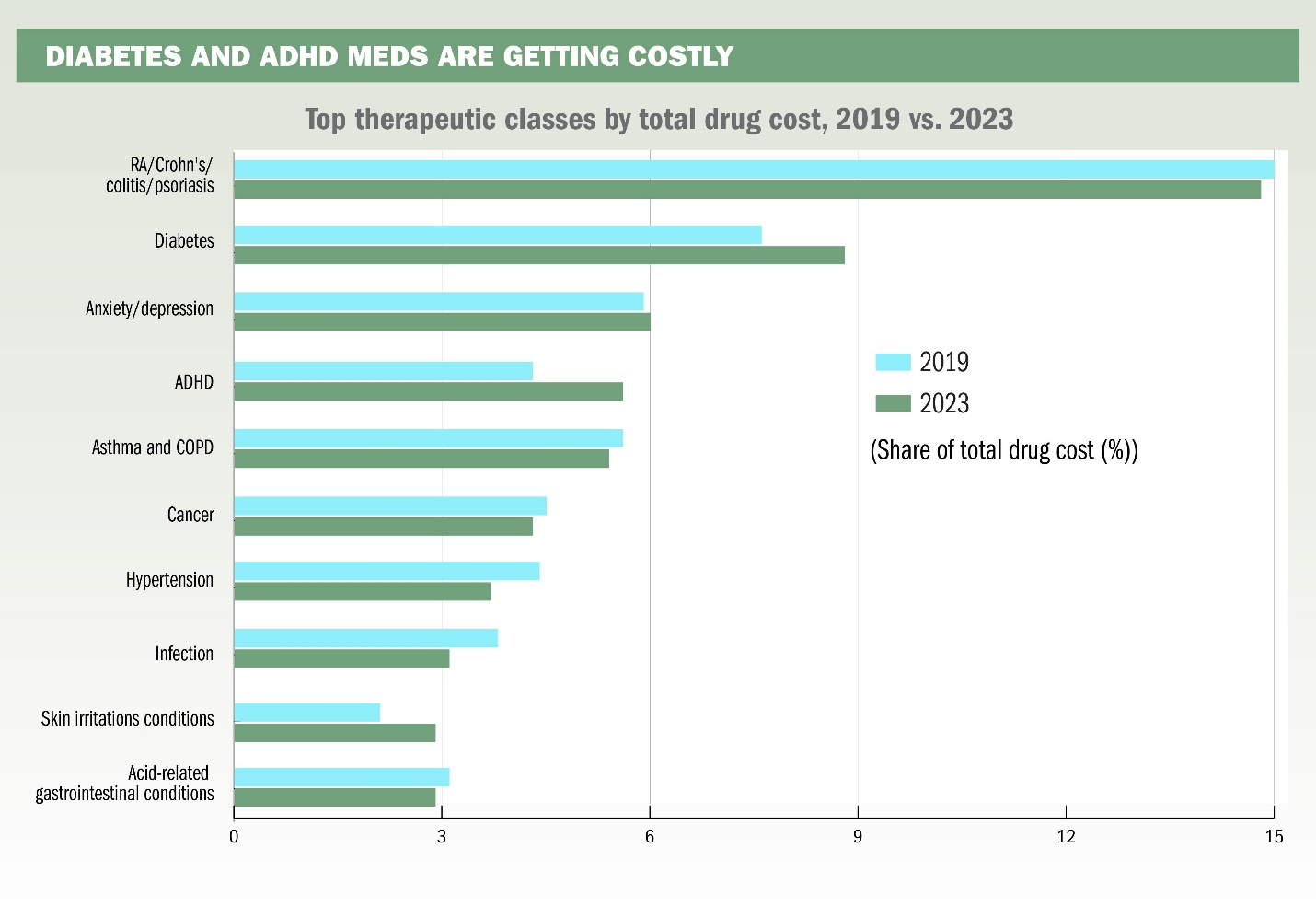
Unsurprisingly, chronic disease is having an increasing impact on both private and public drug plans. Diabetes and weight management emerged as focal points for GreenShield, largely driven by the growing use of GLP-1 medications like Ozempic. Though Ozempic has been on the market since 2018, its use has surged post-COVID. And while the initial growth was explosive, Pojskic notes that usage has started to stabilize.
“There’s more of a stabilization in terms of overall spending, which suggests that most of the patients who have gotten on Ozempic are on it already,” says Pojskic. “It’s not going to disappear anytime soon, but it certainly won't be as explosive as it's been.”
Pojskic is also quick to highlight the potential for generic versions of Ozempic to hit the market in March 2026. While he says there’s no guarantee of this happening, it could provide substantial savings for plan sponsors. New entrants, such as Mounjaro and Zepbound, which promise enhanced efficacy, could also further expand the category.
“When you think about the fact that generics can be upwards of 75 per cent less expensive than their brand counterparts, and Ozempic being a billion-dollar drug in this country, there's a potential for substantial savings in terms of the generic versions of Ozempic," he says.
In addition to the diabetes and weight management trends, the report also points to the continued growth in specialty, high-cost medications as a significant challenge for plan sponsors. These high-cost medications, including biologics for conditions like rheumatoid arthritis and Crohn’s disease, have reshaped drug benefits over the past decade.
The emergence of biosimilars, which are lower-cost alternatives to biologic drugs, has provided plan sponsors with an opportunity to manage these high-cost medications more effectively. Pojskic highlights that Canada has had biosimilars in the market for nearly a decade and have become "a really important driver of the savings that private plans can achieve to be able to afford a lot of these new medications that are coming down the market in the biologic and specialty category."
The rise in medication costs, particularly for specialty and high-cost drugs, is no doubt a conundrum for plan sponsors and employers. After all, plan sponsors face increasing pressure to provide robust coverage while managing costs and will soon have to consider allocating more of their benefits budget towards covering these expenses, as GreenShield highlights. This can lead to a strain on the overall benefits plan, potentially leading to higher premiums or reduced coverage for plan members.
Additionally, the increasing costs of medications can make it difficult for plan sponsors, especially smaller employers, to maintain comprehensive drug coverage for their employees. Organizations will soon be forced to make difficult decisions around plan design, such as increasing deductibles, co-pays, or limiting the number of covered drugs.
Ultimately, group benefits and plan sponsors may benefit from exploring strategies like implementing drug management programs, negotiating better pricing with pharmaceutical companies, and advocating for policy changes to improve drug affordability and access.



